A fast-spreading fungal infection is evolving resistance to common treatments, alarming researchers worldwide.
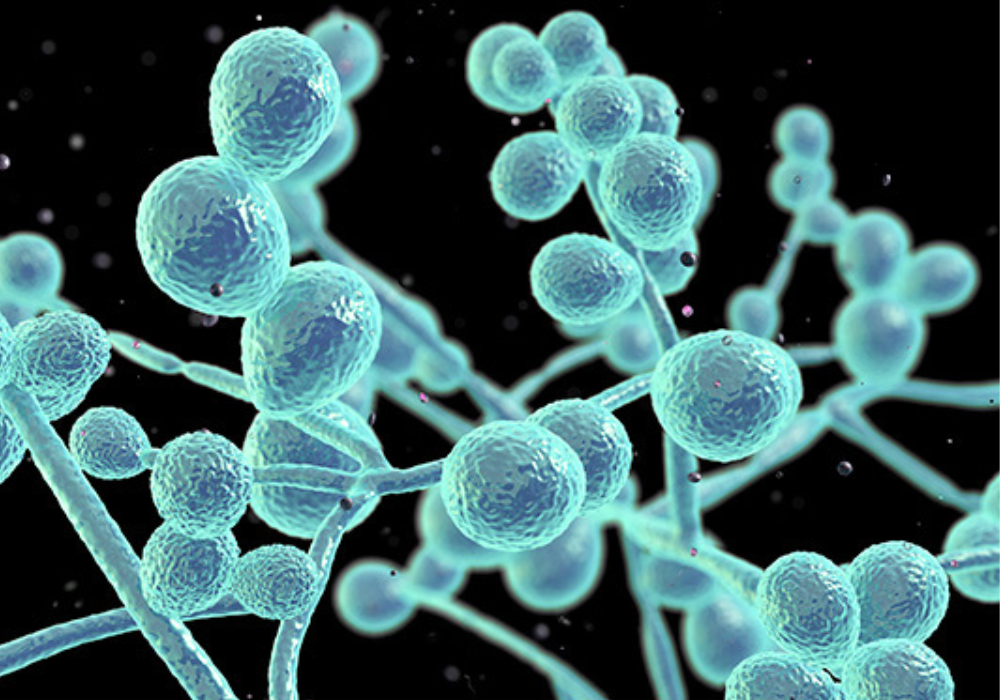
A common fungal infection many take for granted is becoming harder — sometimes impossible — to treat. According to recent research, rising drug resistance in Candida infections (like vaginal or oral thrush) means that standard antifungal medicines are failing more often. Scientists warn that fewer treatment options, persistent recurrences, and increased resistance could turn a once-simple infection into a stubborn, chronic problem. As clinics around the world report rising resistance, experts say it’s time to pay serious attention before a manageable disease becomes a medical nightmare.
1. Thrush Is No Longer Always Easy to Treat

For decades, antifungal drugs like fluconazole reliably cleared up cases of thrush. But now, lab tests show that millions of Candida samples have begun resisting these drugs. This resistance decreases the effectiveness of front-line treatments, making even mild infections harder to kick.
When treatments fail, symptoms can linger or recur — causing physical discomfort, emotional stress, and larger medical bills. For people who experience frequent infections, the loss of reliable treatment is changing thrush from a simple annoyance into a chronic health challenge.
2. Resistance Is Already Widespread in Bloodstream Infections

Drug-resistant Candida isn’t only a problem for superficial infections. Studies now show that bloodstream infections with resistant strains are rising — and those are far more serious. When fungus enters the blood, it can spread to organs and become life-threatening, especially if standard drugs fail.
Because resistance erodes available treatment options, patients with weakened immune systems become highly vulnerable. Doctors warn that invasive fungal diseases once considered manageable may increasingly become dangerous.
3. Mutations, Adaptation, and Biofilms Help Candida Fight Drugs

Candida adapts in multiple ways: genetic mutations change how it reacts to drugs, and some strains create biofilms — slimy layers of fungal cells that protect them like shields. These biofilms block medicines from reaching fungal cells, allowing them to survive doses that would have wiped them out before.
This adaptive ability makes treatment tougher. Even newer antifungals may struggle to penetrate biofilms, and repeated exposure can encourage more resistance. Some scientists now worry that Candida could eventually outsmart most — if not all — standard drugs.
4. Overuse and Misuse of Antifungals Helped Speed Resistance

Like bacteria, fungi can develop resistance when exposed repeatedly or incorrectly to medication. Over-prescription, incomplete treatment courses, or frequent use of antifungal creams can all contribute to resistance build-up.
That means that individuals and healthcare providers both bear responsibility. To preserve the remaining effective drugs, experts urge careful prescribing, stricter guidelines, and public education about how misuse can help dangerous strains evolve.
5. A Shrinking Pool of Effective Drugs Raises Alarm
Unlike antibiotics, there are already very few classes of antifungal drugs — and many of those are losing effectiveness. As resistance rises, doctors may need to rely on older, more toxic medications or new drugs that are still experimental.
This slim drug pipeline means the fungal resistance problem could easily outpace medical solutions. Health experts say development of new antifungals, better diagnostics, and global monitoring should become urgent priorities.
6. Recurring Infections Are Becoming the Norm for Many Patients

Because treatments fail more often, many sufferers now experience recurring bouts of thrush rather than a single, treatable infection. This recurring pattern affects quality of life, self-esteem, and can complicate other health conditions.
Persistent Candida infections also increase the likelihood of resistance spreading — as patients may take repeated or higher doses of drugs. It becomes a vicious cycle, where treatment becomes harder and relapse more likely.
7. Immune-Compromised Patients Face the Highest Risk

People with weakened immune systems — such as those undergoing chemotherapy, living with HIV, or using certain medications — are especially vulnerable. When Candida becomes drug-resistant, their infections are harder to control and more likely to spread.
In some cases, resistant Candida can invade internal organs, leading to serious illness or death. The rising resistance trend is particularly troubling for hospitals and clinics treating immunocompromised patients, requiring heightened vigilance and alternative care strategies.
8. Misdiagnosis and Under-reporting Hide the True Scale of the Problem
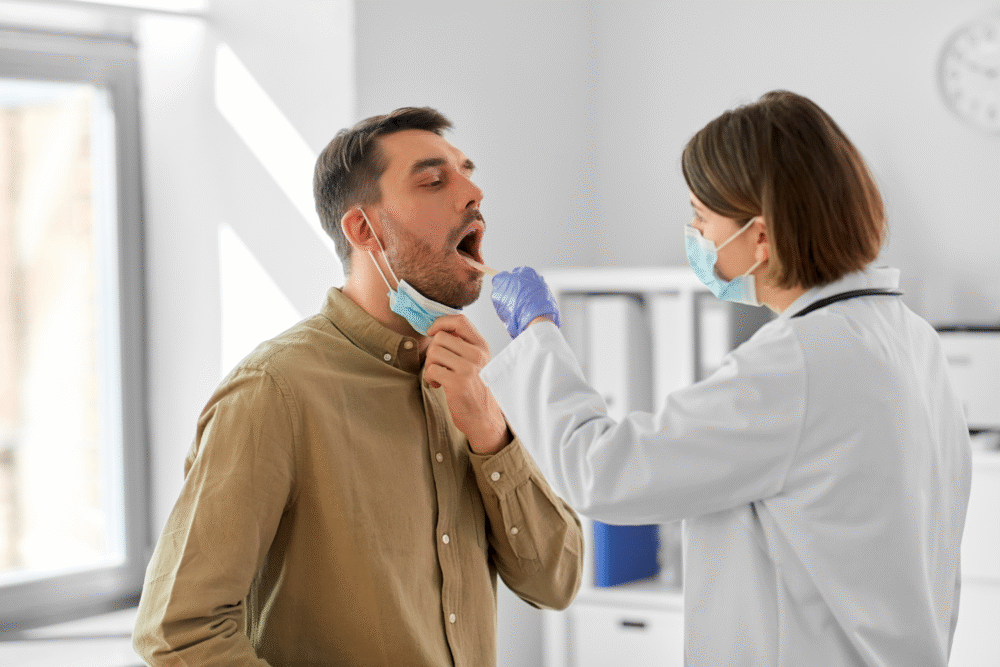
Because Candida infections often resemble other skin or gut conditions, misdiagnosis is common. Laboratories may not test for resistant strains or may lack resources — so many cases likely go unreported.
Low reporting rates hamper public-health efforts to track resistance spread. Without accurate data, it’s harder for researchers to understand trends, allocate resources, or develop targeted responses — giving resistant strains a chance to spread further unnoticed.
9. Resistance Threatens More Than Just Thrush
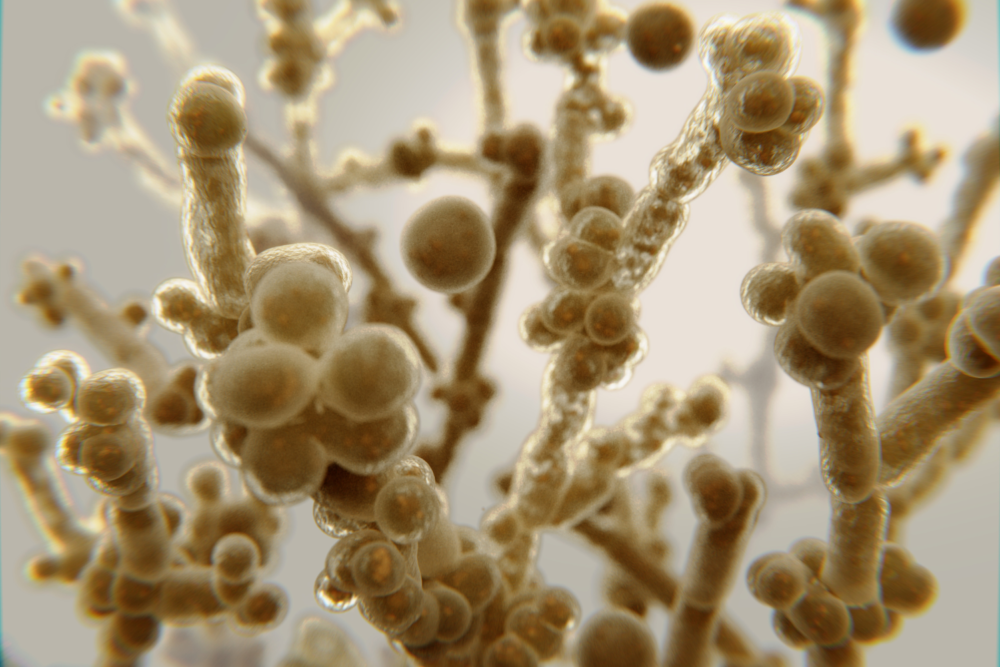
Candida is only one of several fungal pathogens developing drug resistance. Another closely watched species, Candida auris, already causes hard-to-treat, sometimes deadly infections in hospitals. Experts warn that fungal pathogens may become a major global threat alongside antibiotic-resistant bacteria.
A widespread fungal resistance problem could strain healthcare systems, especially as hospital stays, surgical procedures, and immune-compromised patient numbers increase. It could change how we handle infections — and make everyday illnesses far more dangerous.
10. Public Health Experts Call This a Growing Global Crisis

Global health agencies are sounding the alarm: fungal drug resistance should no longer be considered obscure or rare. As resistance spreads across continents, the burden of fungal disease may rise dramatically — particularly in regions with limited healthcare resources.
Experts urge immediate investment in fungal surveillance, drug development, diagnostic technology, and public education. Without swift action, many common fungal infections may become as worrying as bacterial “superbugs.”
11. What You Can Do to Stay Safer Right Now

Individuals can take practical steps to reduce risk: avoid unnecessary antifungal use, complete prescribed treatments fully, maintain good hygiene, and seek medical attention if infections don’t respond to standard drugs. Avoid sharing personal items like towels or razors that can spread Candida.
On a community level, supporting public-health efforts and pushing for better fungal infection awareness helps — because untreated or poorly managed infections benefit resistant strains. Recognizing the threat may be the first step toward keeping this growing problem under control.
