Researchers at MIT and Harvard show donor “natural killer” cells outperform conventional therapies in early cancer trials.
In a breakthrough study led by Massachusetts Institute of Technology and Harvard Medical School researchers, “natural killer” (NK) cells—enhanced immune cells taken from healthy donors—demonstrated superior tumor-killing ability and a safer profile compared with standard treatments in animal models. The team modified the NK cells so they escaped rejection and targeted cancer more precisely. Published in 2025, the work builds on more than 600 NK-cell clinical trials and signals a major shift in cancer immunotherapy.
1. Scientists at MIT and Harvard Develop a New Way to Fight Cancer

A research team from the Massachusetts Institute of Technology and Harvard Medical School has engineered specialized immune cells known as “natural killer” (NK) cells to better identify and destroy cancer cells. The work, published in Nature Biomedical Engineering in 2025, represents a major advancement in immunotherapy.
Unlike chemotherapy or radiation, this approach uses the body’s own immune mechanisms to attack tumors while leaving healthy tissue unharmed, reducing the severe side effects seen in many cancer treatments.
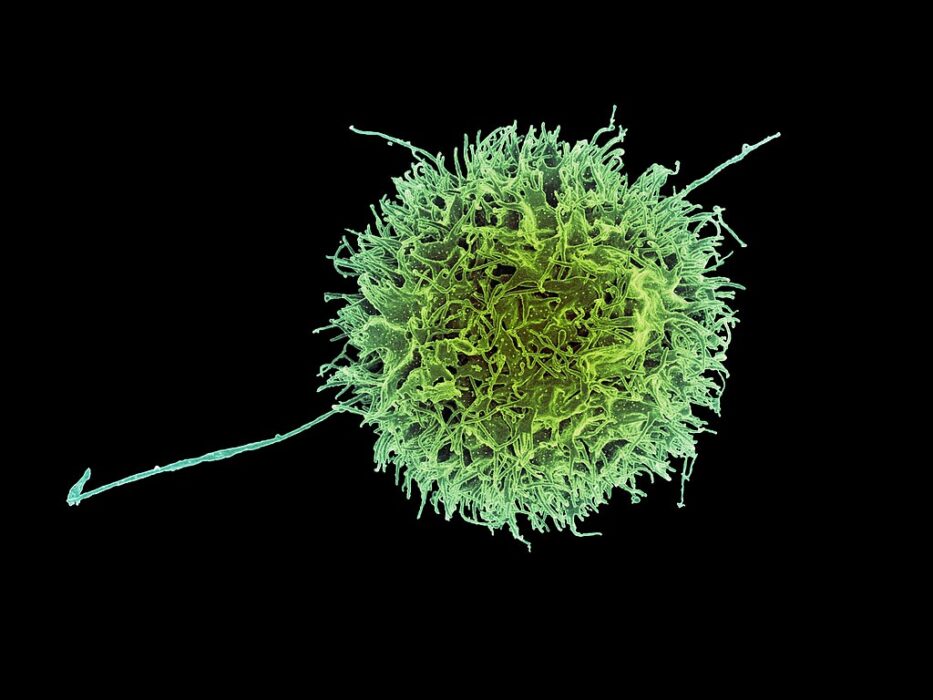
2. Natural Killer Cells Are the Immune System’s First Line of Defense

NK cells are a type of white blood cell that act quickly against viruses and abnormal cells, including early-stage cancers. They patrol the body, identifying and eliminating cells that show signs of infection or genetic damage.
Scientists have long known about their cancer-fighting potential, but these cells are difficult to produce in large numbers and often lose effectiveness inside the tumor environment—a challenge researchers at MIT and Harvard set out to overcome.
3. Researchers Engineered Donor Cells to Be “Universal” and Non-Rejectable

The new therapy uses NK cells from healthy donors rather than relying solely on a patient’s own immune system. The team genetically modified these donor cells so they would not be rejected by the recipient’s immune defenses.
This breakthrough means NK cells could one day be “off-the-shelf” treatments—ready for use when needed, rather than custom-built for each patient. That could dramatically lower costs and speed up cancer therapy timelines.
4. Modified Cells Target Cancer More Precisely
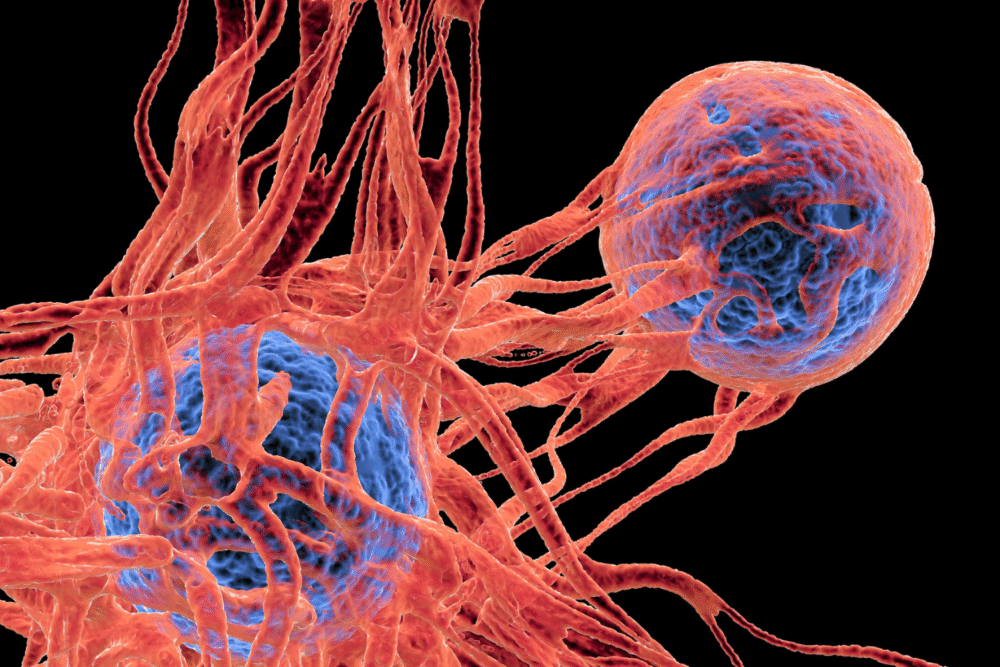
The MIT–Harvard team equipped the NK cells with molecular receptors designed to recognize specific proteins on cancer cell surfaces. These receptors act like guided missiles, improving the precision of tumor targeting.
In lab experiments, the engineered NK cells sought out and destroyed cancer cells while leaving healthy cells untouched. The precision could reduce the collateral damage often caused by chemotherapy and radiation, which harm both malignant and normal tissues.
5. Early Tests Show Greater Effectiveness Than Standard Treatments

In preclinical models, the modified NK cells outperformed traditional therapies in shrinking or eliminating tumors. The cells persisted longer in the body, maintained higher activity levels, and caused fewer toxic side effects.
Researchers compared their results with current chemotherapy standards and found that tumor reduction was faster and more complete in animals treated with engineered NK cells. Human trials are now being prepared to evaluate safety and effectiveness in patients.
6. The Treatment Could Help Patients Resistant to Other Therapies

Some cancers, such as solid tumors in the pancreas, lungs, or brain, resist traditional immunotherapies that depend on T cells. NK cells may offer an alternative route because they can recognize and attack cancer cells without needing prior exposure.
This independence from conventional immune signaling makes NK-based therapy promising for patients whose cancers have stopped responding to existing treatments, offering new hope in previously untreatable cases.
7. A Safer Approach With Fewer Toxic Side Effects

Chemotherapy and some immunotherapies can damage bone marrow, trigger inflammation, or cause severe fatigue. In contrast, NK-cell therapy appears to avoid many of these issues. Because NK cells naturally regulate immune activity, they pose less risk of causing autoimmune complications.
In mouse studies, recipients of engineered NK cells showed minimal toxicity and recovered quickly, suggesting the therapy could be both safer and better tolerated than conventional cancer drugs.
8. Natural Killer Cells Could Work Alongside Other Immunotherapies
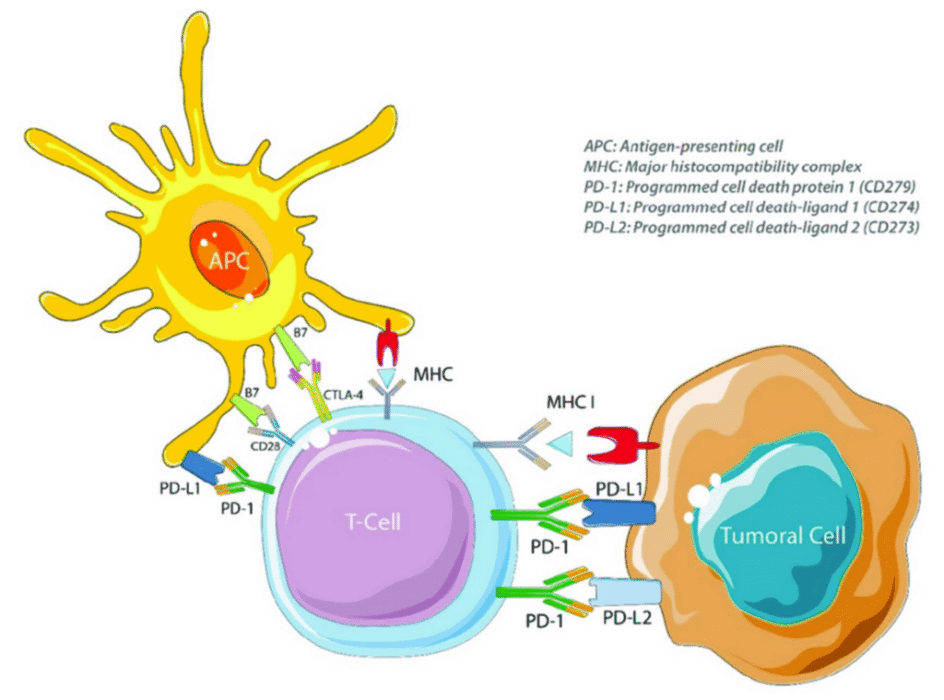
Researchers believe NK cells might complement other cancer treatments rather than replace them entirely. By combining NK-cell therapy with checkpoint inhibitors or targeted drugs, scientists hope to achieve stronger, longer-lasting tumor control.
Clinical trials are already exploring how engineered NK cells interact with these existing therapies. If results continue to show synergy, future cancer treatment may rely on tailored combinations rather than single-drug approaches.
9. Manufacturing Advances Make Large-Scale Therapy Possible

One of the biggest challenges in immunotherapy is producing enough cells for patients. The MIT and Harvard scientists developed a method to grow and multiply NK cells efficiently in the lab using bioreactors that preserve their killing ability.
This scalable process could make NK-cell therapies more accessible, reducing dependence on costly, individualized manufacturing—a barrier that has slowed the rollout of other advanced cell-based treatments.
10. The Discovery Builds on Decades of NK-Cell Research
The breakthrough didn’t happen overnight. Scientists have studied NK cells since the 1970s, but only in the past decade have gene-editing tools like CRISPR and synthetic biology allowed them to fine-tune the cells’ behavior.
More than 600 NK-cell clinical trials are underway globally, exploring their use in leukemia, lymphoma, and solid tumors. The new MIT–Harvard research provides one of the strongest proofs yet that NK cells can outperform traditional therapies.
11. Clinical Trials Will Determine Safety and Long-Term Benefits

Before approval for widespread use, the therapy must pass through rigorous human testing. Early-stage clinical trials are expected to begin in 2025, focusing first on safety and dosage.
Researchers plan to monitor whether the modified NK cells remain active over time and whether they can fully eradicate tumors in humans as they did in lab studies. Success could pave the way for a new class of immune-based cancer treatments.
12. Scientists See This as a Turning Point in Cancer Treatment

Experts describe the findings as a milestone in the evolution of immunotherapy. By creating a therapy that’s both potent and well-tolerated, researchers believe NK cells could one day rival T-cell–based treatments like CAR-T therapy.
The long-term goal is to make these engineered immune cells readily available to hospitals worldwide. If clinical results match current research, NK-cell therapy could become one of the safest and most effective cancer treatments of the next decade.
