These pandemics didn’t just spread disease—they reshaped culture, power, and history.
Historic pandemics have repeatedly transformed societies in deep and lasting ways, influencing population dynamics, economies, and governance. Experts at the Centers for Disease Control and Prevention say understanding these events sheds light on how infectious diseases interact with social structures and public health responses.
From ancient plagues to modern outbreaks, studying the evolution of containment measures and vaccination efforts reveals critical lessons for effectively managing today’s health challenges.
1. The Black Death radically altered Europe’s population and social structure.

The Black Death, which swept through Europe in the 14th century, wiped out nearly a third of the population, deeply affecting society. This pandemic reshaped economic structures, leading to labor shortages and higher wages for workers.
Social hierarchies shifted as the immense loss of life challenged the power of feudal lords. With fewer mouths to feed, food demand decreased, stimulating economic changes. This era highlights the transformative impact pandemics can have on social and economic dynamics, illustrating the importance of adaptive societal responses.
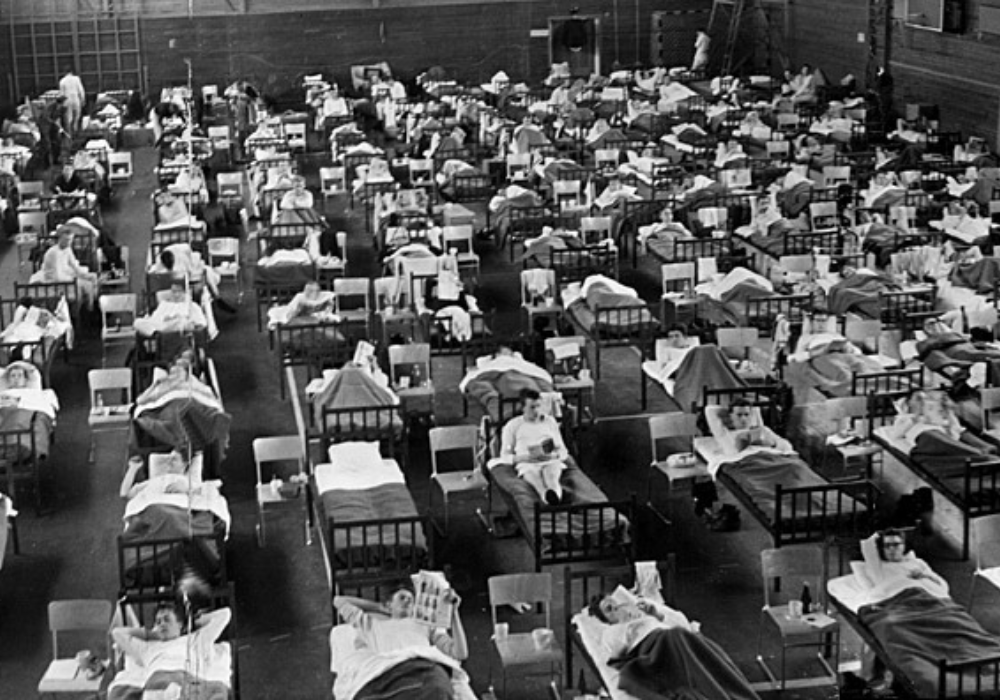
2. The Spanish Flu spread worldwide, causing massive global casualties.

The Spanish Flu of 1918-1919 infected an estimated one-third of the global population, with a staggering death toll worldwide. Unlike other pandemics, its rapid spread occurred at the end of World War I, exacerbating global instability. Quarantine measures, though challenging to implement, became essential in managing public health.
Communities had to adapt swiftly, leading to better understanding of influenza and its transmission. This crisis underscored the necessity for effective public health responses and adaptations, many principles of which continue to guide pandemic management today.
3. The Plague of Justinian severely weakened the Byzantine Empire.

Between 541 and 542 AD, the Plague of Justinian struck the Byzantine Empire, severely crippling its strength by decimating the population, particularly in urban centers. This pestilence significantly weakened military forces and disrupted agriculture, leading to food shortages and economic turmoil.
The Byzantine Empire struggled to rebound, marking the beginning of its decline. This pandemic illustrated how infectious diseases can dramatically affect political stability, military might, and economic health, offering insights into the vulnerabilities of interconnected societies to such disruptions.
4. The Asian Flu sparked major public health reforms across continents.
In 1957, the Asian Flu emerged, becoming a global concern and prompting sweeping public health reforms. As the flu spread, governments recognized the need for coordinated responses, improving surveillance and international communication. Vaccination campaigns were swiftly organized, setting new standards for future disease outbreaks.
This pandemic taught valuable lessons about the importance of rapid intervention and collaboration across nations, leading to more robust health systems prepared to manage widespread health threats with efficiency and effectiveness.
5. The Antonine Plague devastated the Roman Empire’s military forces.
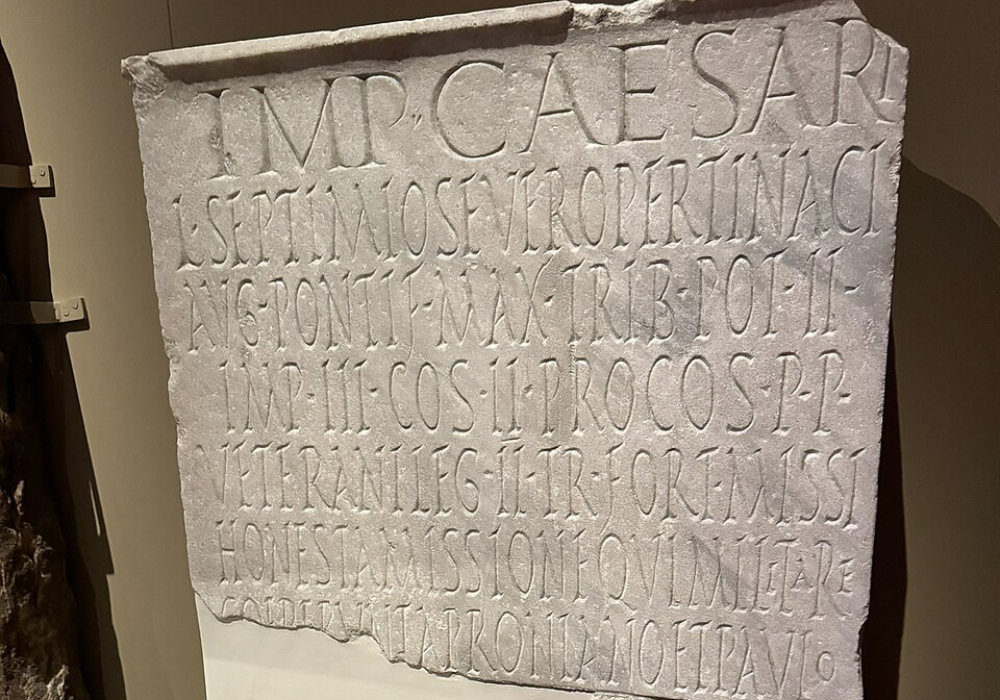
The Antonine Plague, hitting the Roman Empire from 165 to 180 AD, crippled its military capabilities, deeply affecting its ability to defend its territories. Estimated to have killed millions, it seriously depleted the ranks of Roman soldiers.
The Empire faced economic and social strain as resources were diverted toward disease management. This plague revealed the vulnerability of even powerful states to health crises, reminding societies of the need to incorporate public health strategies into their stability and security frameworks.
6. The Third Cholera Pandemic changed sanitation and water supply systems.
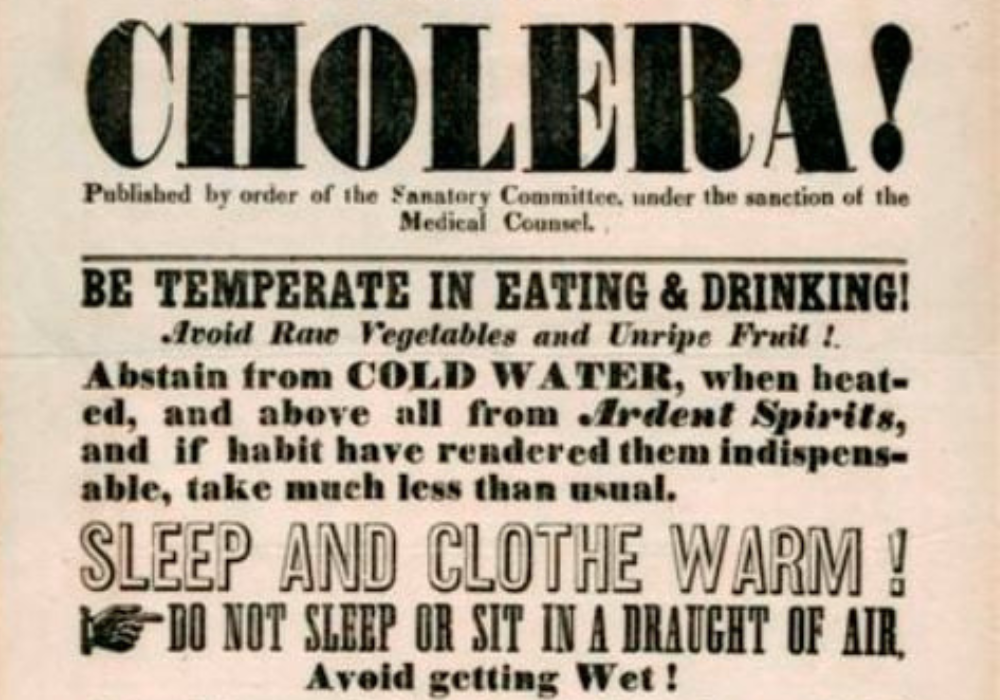
During the Third Cholera Pandemic of the mid-19th century, societies recognized the importance of sanitation in combating disease. This cholera outbreak spurred significant changes in water supply and waste management systems, especially in urban areas. Improved understanding of waterborne diseases led to innovations such as sanitary sewer systems.
These infrastructure developments drastically reduced water contamination, promoting overall better public health. This historic health crisis underscored the role of proper sanitation in preventing disease spread and fostering healthier living conditions.
7. The HIV/AIDS crisis transformed global attitudes toward public health.

The onset of the HIV/AIDS crisis in the late 20th century prompted a transformative shift in global public health strategies and societal attitudes. As the virus spread, widespread misinformation and stigma highlighted the need for better education and empathy. The crisis led to the development of targeted awareness campaigns and advancements in antiretroviral treatments.
Public health systems strengthened their focus on prevention and care, emphasizing a more inclusive approach to health care access and support for affected communities.
8. The Smallpox epidemics decimated indigenous populations in the Americas.

Smallpox epidemics, brought by European colonizers, led to the catastrophic decline of indigenous populations in the Americas. Lacking immunity, these communities faced devastating mortality rates, which led to cultural and societal collapse. The effect of these outbreaks reshaped the demographic and cultural landscapes significantly.
It was a tragic chapter that emphasizes the impact of infectious disease in historical contexts, highlighting the need for mindful cross-cultural interactions and recognizing the profound influence of disease on human societies across continents.
9. The Russian Flu influenced early 20th-century medical response strategies.

In 1889-1890, the Russian Flu pandemic challenged early medical response strategies and influenced future public health planning. Limited medical knowledge at the time led to varied responses to containing the virus, resulting in significant disease spread and mortality.
The flu pandemic highlighted shortcomings in disease detection and spurred progress in understanding respiratory pathogens. The Russian Flu’s legacy is reflected in the improvement of healthcare systems and increased responsiveness, offering insights that guided later approaches to global health challenges.
10. The SARS outbreak accelerated innovations in disease detection worldwide.
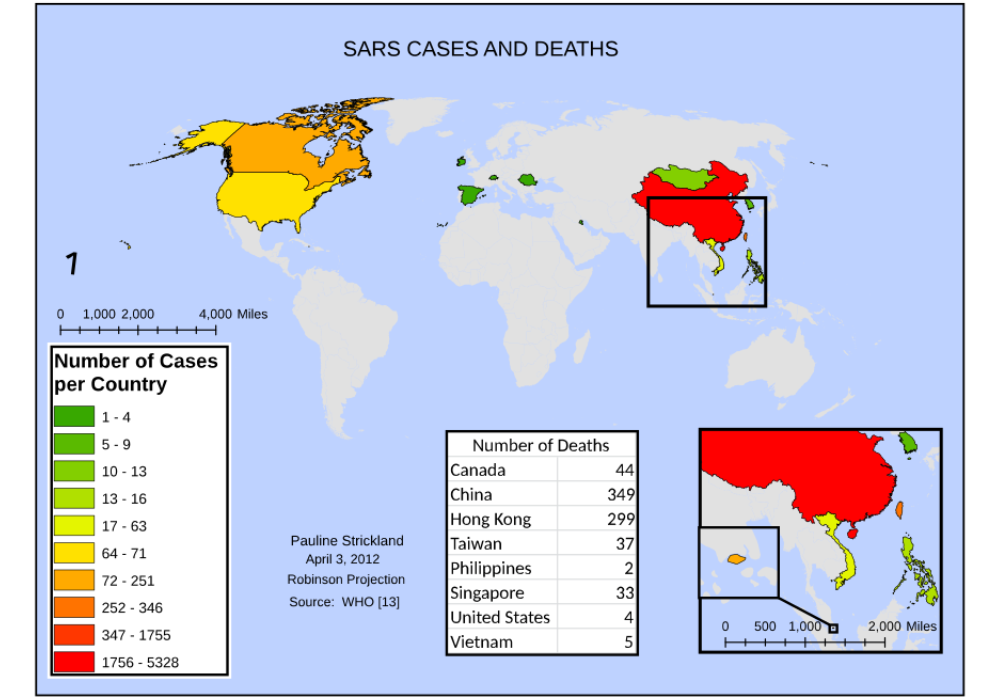
The SARS outbreak of 2002-2003 propelled advancements in real-time disease detection and monitoring technology. As the virus spread across Asia and beyond, health authorities embraced modern surveillance tools to track infections and containment efforts. It led to more integrated global health networks and the early identification of emerging threats.
SARS emphasized the critical importance of rapid information sharing and solidified the role of technology in enhancing public health capabilities, laying the groundwork for future pandemic preparedness.
11. The Hong Kong Flu triggered improvements in vaccine development processes.

The Hong Kong Flu pandemic of 1968 accelerated developments in vaccine technology, as nations strove to protect their populations from the new strain. With millions affected globally, emergent vaccine production techniques were tested and refined. These innovations allowed for more efficient and timely distribution, setting a new benchmark for flu vaccine readiness.
This pandemic underscored the vital role of scientific progress in combating infectious diseases, leading to more structured and responsive vaccination strategies in the subsequent decades.
12. The MERS outbreak heightened awareness of zoonotic disease transmission.
The MERS outbreak in 2012 heightened global awareness of zoonotic diseases, furthering research into how animal pathogens jump to humans. As MERS spread, understanding zoonoses became a priority, leading to increased surveillance and research on interspecies virus transmission.
Monitoring animal health has since become crucial in preventing human epidemics. The comprehensive study of such diseases has informed guidelines that shape current and future public health strategies, effectively and proactively addressing cross-species transmission risks.
